Managing risk within hospitals is not only essential for patient safety but also for upholding compliance and stability across all organizational levels. By proactively identifying and addressing potential hazards, hospitals can prevent adverse events and create a safer environment for patients and staff. A critical method for reducing hospital liabilities involves leveraging comprehensive solutions such as Coverys liability insurance, which can support risk transfer and provide reassurance for hospital administrators in mitigating unforeseen risks.
Today’s evolving healthcare landscape demands intricate layers of risk management, spanning clinical processes, technology, staff preparedness, and regulatory adherence. Efficient strategies combine advanced tools, integrated teams, and targeted education, promoting proactive incident prevention and resilience in the face of emergencies. Realizing such a robust framework not only averts costly disruptions but also positions hospitals to provide consistently high-quality care.
Establishing and maintaining these layers requires ongoing adaptation and a culture that values transparency, accountability, and collaboration across all departments. With increasingly digitized systems and complex public health threats, hospitals must remain vigilant by constantly modernizing their risk mitigation approaches. Sustaining these practices helps organizations react swiftly to emergencies, optimize workflows, and protect sensitive patient data from potential breaches. Equipping hospital teams to anticipate and address risks before they escalate is paramount for operational continuity and public trust.
Additionally, exploring best practices from leading healthcare organizations and evidence-based guidelines can further reinforce a hospital’s preparedness for both clinical and administrative challenges.
Establishing a Risk Management Team
At the heart of every robust hospital risk strategy lies a specialized and multidisciplinary risk management team. This core group should comprise representatives from across clinical, operational, and administrative departments, including infection prevention, emergency management, nursing, pharmacy, and other relevant areas. Their coordinated expertise guides the creation and implementation of risk plans, ensures compliance with national standards, and drives the education and empowerment of all staff. Hospitals with dedicated teams are far better poised to identify gaps proactively and to respond to evolving threats with speed and cohesion.
Leveraging Technology for Risk Mitigation
Technology plays a pivotal role in modern risk management. The widespread adoption of electronic health records (EHRs) minimizes documentation errors and promotes reliable tracking of patient care. Automated systems and monitoring tools generate real-time alerts for deviations from protocols or adverse events, enabling immediate corrective action. Artificial intelligence (AI) can proactively identify emerging patterns or near misses, acting as a continuous safety net, which empowers hospitals to intervene well before incidents escalate to reportable levels. Leveraging tech-based solutions provides an ongoing advantage in both quality improvement and risk avoidance.

Staff Training and Education
Ongoing education is essential to keep clinical and non-clinical staff prepared for risk scenarios. Workshop sessions, e-learning modules, and simulation drills provide team members with hands-on experience in managing real-time healthcare emergencies, infectious disease outbreaks, and patient safety issues. An adaptable workforce is one of the most effective barriers against adverse outcomes, ensuring risk management protocols are not merely policies on paper but are ingrained in everyday practice.
Fostering a Culture of Safety
Cultivating a strong culture of safety means establishing an environment where staff are encouraged to report errors, openly discuss potential risks, and actively participate in improvement initiatives—without fear of blame or reprisal. This climate fosters accountability and continuous learning, laying the groundwork for ongoing improvements in patient and workforce safety. Celebrating team members’ efforts to escalate and resolve risks reinforces the organization’s commitment to best practices and shared responsibility.
Developing Emergency Preparedness Plans
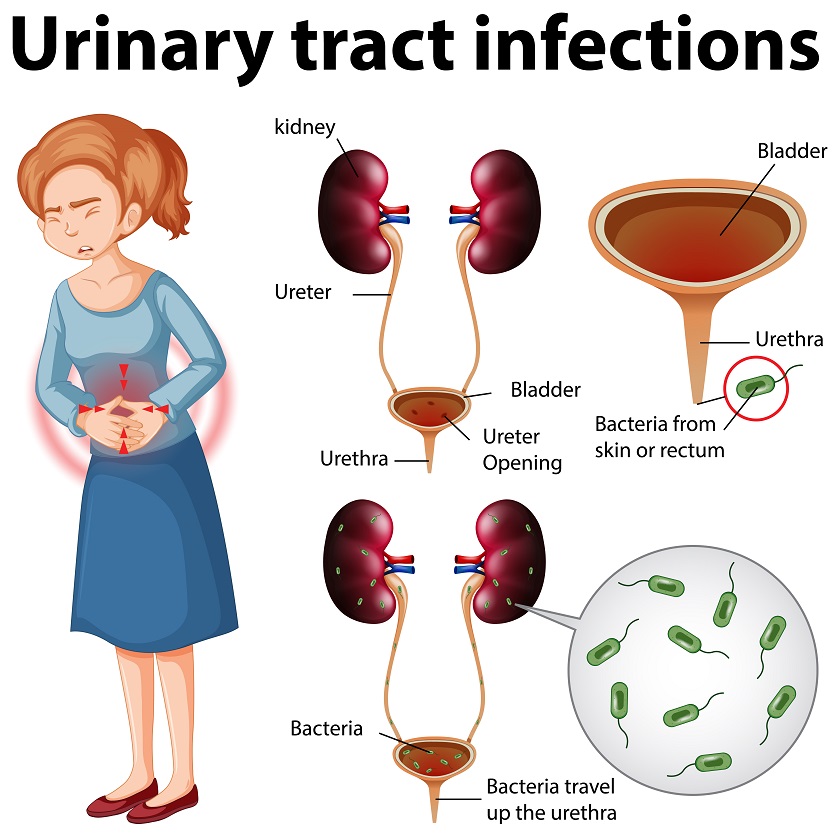
Hospitals must maintain thorough emergency preparedness plans to rapidly respond to public health threats, natural disasters, or pandemics. These plans should be regularly reassessed and updated based on current hazard assessments, surveillance results, and new best practices. Involving an infectious disease task force or crisis management committee strengthens the hospital’s ability to adapt and coordinate during high-consequence scenarios. Reliable communication protocols and inventory management ensure that resources are allocated quickly and efficiently when every minute counts.
Implementing Cybersecurity Measures
The transition to digital health records and interconnected networks has made healthcare a significant target for cybercriminals. Hospitals must therefore establish robust cybersecurity protocols, including regular risk assessments, mobile device management, and dedicated teams to monitor for vulnerabilities. Hospitals should also draft and rehearse cyber incident response plans so staff can act decisively if digital infrastructure is compromised. Engaging in industry-wide information-sharing platforms enhances their ability to stay ahead of emerging threats.
Conducting Regular Audits and Assessments
Routine audits—spanning patient safety, clinical practice, and technology infrastructure—are indispensable for ongoing risk reduction. These reviews highlight compliance gaps, staff training needs, or systemic vulnerabilities, yielding actionable data for rapid intervention. The audit process should be constructive, aimed at promoting continuous learning and transparent improvement rather than penalizing individual missteps.
Collaborating with Public Health Agencies
Collaboration with public health agencies helps hospitals stay updated with regulations and access emergency support. Strong partnerships enable swift info sharing, standardize processes, and incorporate guidelines into hospital operations. Integrating preparedness and surveillance improves resilience and response. Embedding risk strategies boosts patient safety, ensures compliance, and builds trust. Regular review of these approaches is vital for a resilient healthcare system.
Conclusion: Building Resilient and Safe Healthcare Systems
Effective hospital risk management is not a one-time initiative but a dynamic, organization-wide commitment to safety, preparedness, and continuous improvement. By uniting multidisciplinary expertise, leveraging technology, and fostering a culture of transparency and accountability, hospitals can proactively address potential threats before they escalate. Ongoing staff education, collaboration with public health partners, and rigorous audits further strengthen institutional resilience. When emergency readiness and cybersecurity are prioritized alongside patient care, healthcare organizations not only protect their operations but also uphold the highest standards of safety, trust, and quality for every patient they serve.